Abstract
Purpose
This study aimed to explore the relationship between oral contraceptive use and blood pressure values and in a national cohort of women adolescents and to investigate the level of coexistence of the high blood pressure levels, dyslipidemia or insulin resistance.
Methods
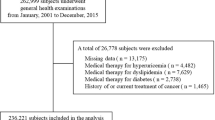
This is a retrospective cohort study that evaluated data form 14,299 adolescents aged 14 to 17 years. Crude and race-and age-adjusted analyses were performed using Poisson regression to estimate the prevalence ratios. Data clustering analysis was performed using machine learning approaches supported by an unsupervised neural network of self-organizing maps.
Results
We found that 14.5% (n = 2076) of the women adolescents use oral contraceptives. Moreover, an increased prevalence of high blood pressure, dyslipidemia, and insulin resistance (all P < 0.001) was observed among adolescents who use oral contraceptives as compared to those who do not. Our analysis also showed that 2.3% of adolescents using oral contraceptives had both high blood pressure levels and dyslipidemia, whereas 3.2% had high blood pressure levels combined with insulin resistance (all P < 0.001). The algorithmic investigative approach demonstrated that total cholesterol, LDLc, HDLc, insulin, and HOMA-IR were the most predicted variables to assist classificatory association in the context of oral contraceptive use among women adolescents with high blood pressure.
Conclusions
These findings suggest that oral contraceptives were associated with an increased prevalence of high blood pressure, dyslipidemia, and insulin resistance among women adolescents. Although the indication of this therapy is adequate to avoid unintended pregnancies, their use must be based on rigorous individual evaluation and under constant control of the cardiometabolic risk factors.

Similar content being viewed by others
Data availability
Not applicable.
References
Borges AL, Fujimori E, Kuschnir MC, Chofakian CB, de Moraes AJ, Azevedo GD et al (2016) ERICA sexual initiation and contraception in Brazilian adolescents. Rev Saude Publica 50:15s. https://doi.org/10.1590/S01518-8787.2016050006686
Todd N, Black A (2020) Contraception for Adolescents. J Clin Res Pediatr Endocrinol 12:28–40. https://doi.org/10.4274/jcrpe.galenos.2019.2019.S0003
Brynhildsen J (2014) Combined hormonal contraceptives: prescribing patterns, compliance, and benefits versus risks. Therapeutic advances in drug safety 5:201–213. https://doi.org/10.1177/2042098614548857
Williams WV (2017) Hormonal contraception and the development of autoimmunity: a review of the literature. Linacre Q 84:275–295. https://doi.org/10.1080/00243639.2017.1360065
Godsland IF (2005) Oestrogens and insulin secretion. Diabetologia 48:2213–2220. https://doi.org/10.1007/s00125-005-1930-0
Lalude OO (2013) Risk of cardiovascular events with hormonal contraception: insights from the Danish cohort study. Curr Cardiol Rep 15:374. https://doi.org/10.1007/s11886-013-0374-2
Liu H, Yao J, Wang W, Zhang D (2017) Association between duration of oral contraceptive use and risk of hypertension: a meta-analysis. J Clin Hypertens (Greenwich) 19:1032–1041. https://doi.org/10.1111/jch.13042
Steenland MW, Zapata LB, Brahmi D, Marchbanks PA, Curtis KM (2013) Appropriate follow up to detect potential adverse events after initiation of select contraceptive methods: a systematic review. Contraception 87:611–624. https://doi.org/10.1016/j.contraception.2012.09.017
Gourdy P, Bachelot A, Catteau-Jonard S et al (2012) Hormonal contraception in women at risk of vascular and metabolic disorders: guidelines of the French Society of Endocrinology. Ann Endocrinol (Paris) 73:469–487. https://doi.org/10.1016/j.ando.2012.09.001
Nawrot TS, Den Hond E, Fagard RH, Hoppenbrouwers K, Staessen JA (2003) Blood pressure, serum total cholesterol and contraceptive pill use in 17-year-old girls. Eur J Cardiovasc Prev Rehabil 10:438–442. https://doi.org/10.1097/01.hjr.0000103463.31435.1e
Le-Ha C, Beilin LJ, Burrows S, Huang RC, Oddy WH, Hands B, Mori TA (2013) Oral contraceptive use in girls and alcohol consumption in boys are associated with increased blood pressure in late adolescence. Eur J Prev Cardiol 20:947–955. https://doi.org/10.1177/2047487312452966
Lewandowski SK, Duttge G, Meyer T (2020) Quality of life and mental health in adolescent users of oral contraceptives. Results from the nationwide, representative German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Qual Life Res 29:2209–2218. https://doi.org/10.1007/s11136-020-02456-y
Kharbanda EO, Parker ED, Sinaiko AR, Daley MF, Margolis KL, Becker M et al (2014) Initiation of oral contraceptives and changes in blood pressure and body mass index in healthy adolescents. J Pediatr 165:1029–1033. https://doi.org/10.1016/j.jpeds.2014.07.048
Bloch KV, Szklo M, Kuschnir MC, Abreu Gde A, Barufaldi LA, Klein CH et al (2015) The Study of Cardiovascular Risk in Adolescents–ERICA: rationale, design and sample characteristics of a national survey examining cardiovascular risk factor profile in Brazilian adolescents. BMC Public Health 15:94. https://doi.org/10.1186/s12889-015-1442-x
Souza AA, Almeida DC, Barcelos TS, Bortoletto RC, Munoz R, Waldman H et al (2021) Simple hemogram to support the decision-making of COVID-19 diagnosis using clusters analysis with self-organizing maps neural network. Soft comput 17:1–12. https://doi.org/10.1007/s00500-021-05810-5
Darroch JE, Woog V, Bankole A, Ashford L (2016) Adding it up: costs and benefits of meeting the contraceptive needs of adolescents, New York: Guttmacher Institute, 2016. Guttmacher Institute. https://www.guttmacher.org/report/adding-it-meeting-contraceptive-needs-of-adolescents
Park H, Kim K (2013) Associations between oral contraceptive use and risks of hypertension and prehypertension in a cross-sectional study of Korean women. BMC Womens Health 13:39. https://doi.org/10.1186/1472-6874-13-39
Goldhaber SZ, Hennekens CH, Spark RF, Evans DA, Rosner B, Taylor JO et al (1984) Plasma renin substrate, renin activity, and aldosterone levels in a sample of oral contraceptive users from a community survey. Am Heart J 107:119–122. https://doi.org/10.1016/0002-8703(84)90144-3
Chen JT, Kotani K (2012) Oral contraceptive therapy increases oxidative stress in pre-menopausal women. Int J Prev Med 3:893–896. https://doi.org/10.4103/2008-7802.104862
Josse AR, Garcia-Bailo B, Fischer K, El-Sohemy A (2012) Novel effects of hormonal contraceptive use on the plasma proteome. PLoS ONE 7:e45162. https://doi.org/10.1371/journal.pone.0045162
Naz F, Jyoti S, Akhtar N, Afzal M, Siddique YH (2012) Lipid profile of women using oral contraceptive pills. Pak J Biol Sci 15:947–950. https://doi.org/10.3923/pjbs.2012.947.950
Momeni Z, Dehghani A, Fallahzadeh H, Koohgardi M, Dafei M, Hekmatimoghaddam SH et al (2020) The impacts of pill contraceptive low-dose on plasma levels of nitric oxide, homocysteine, and lipid profiles in the exposed vs. non exposed women: as the risk factor for cardiovascular diseases. Contracept Reprod Med 5:7
Palmisano BT, Zhu L, Stafford JM (2017) Role of Estrogens in the regulation of liver lipid metabolism. Adv Exp Med Biol 1043:227–256. https://doi.org/10.1007/978-3-319-70178-3_12
Frempong BA, Ricks M, Sen S, Sumner AE (2008) Effect of low-dose oral contraceptives on metabolic risk factors in African-American women. J Clin Endocrinol Metab 93(6):2097–2103. https://doi.org/10.1210/jc.2007-2599
Deleskog A, Hilding A, Östenson CG (2011) Oral contraceptive use and abnormal glucose regulation in Swedish middle aged women. Diabetes Res Clin Pract 92:288–292. https://doi.org/10.1016/j.diabres.2011.02.014
Cortés ME, Alfaro AA (2014) The effects of hormonal contraceptives on glycemic regulation. Linacre Q 81:209–218. https://doi.org/10.1179/2050854914Y.0000000023
Ginsberg HN, Zhang YL, Hernandez-Ono A (2005) Regulation of plasma triglycerides in insulin resistance and diabetes. Arch Med Res 36:232–240. https://doi.org/10.1016/j.arcmed.2005.01.005
Tricò D, Natali A, Mari A, Ferrannini E, Santoro N, Caprio S (2018) Triglyceride-rich very low-density lipoproteins (VLDL) are independently associated with insulin secretion in a multiethnic cohort of adolescents. Diabetes Obes Metab 20:2905–2910. https://doi.org/10.1111/dom.13467
Funding
This research is not funded by a specific project.
Author information
Authors and Affiliations
Contributions
P.X.A. and M.C.F. were responsible for article conceptualization. P.X.A. and P.M. made the literature search and prepared the tables. D.C.A. and A.A.S. made the neural network of self-organizing maps. All authors wrote the main manuscript text. All authors were responsible for data curation, drafting, and approval of the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
All participants signed an informed consent form at the time of enrollment. The study was approved by the Research Ethics Committee of the head institution of the national database center (IESC/UFRJ—Process 45/2008) and the accomplishment of the current study was approved by the Research Ethics Committee of the Federal University of São Paulo (Approval Number: 3.007.121).
Consent for publication
All authors read and approve the manuscript and give their consent for submission and publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Araújo, P.X., Moreira, P., de Almeida, D.C. et al. Oral contraceptives in adolescents: a retrospective population-based study on blood pressure and metabolic dysregulation. Eur J Clin Pharmacol (2024). https://doi.org/10.1007/s00228-024-03671-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00228-024-03671-z