Abstract
Background and Objective
Adverse drug events (ADEs) are becoming a significant public health issue. However, reports on ADE-related mortality are limited to national-level evaluations. Therefore, we aimed to reveal overall trends in ADE-related mortality across the 21st century on an international level.
Methods
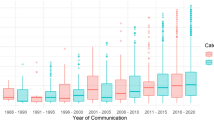
This observational study analysed long-term trends in ADE-related mortality rates from 2001 to 2019 using the World Health Organization Mortality Database. The rates were analysed according to sex, age and region. North America, Latin America and the Caribbean, Western Europe, Eastern Europe and Western Pacific regions were assessed. Fifty-four countries were included with four-character International Statistical Classification of Disease and Related Health Problems, Tenth Revision codes in the database, population data in the World Population Prospects 2019 report, mortality data in more than half of the study period, and high-quality or medium-quality death registration data. A locally weighted regression curve was used to show international trends in age-standardised rates.
Results
The global ADE-related mortality rate per 100,000 population increased from 2.05 (95% confidence interval 0.92–3.18) in 2001 to 6.86 (95% confidence interval 5.76–7.95) in 2019. Mortality rates were higher among men than among women, especially in those aged 20–50 years. The population aged ≥ 75 years had higher ADE-related mortality rates than the younger population. North America had the highest mortality rate among the five regions. The global ADE-related mortality rate increased by approximately 3.3-fold from 2001 to 2019.
Conclusions
The burden of ADEs has increased internationally with rising mortality rates. Establishing pharmacovigilance systems can facilitate efforts to reduce ADE-related mortality rates globally.



Similar content being viewed by others
References
Falconer N, Barras M, Martin J, Cottrell N. Defining and classifying terminology for medication harm: a call for consensus. Eur J Clin Pharmacol. 2019;75:137–45. https://doi.org/10.1007/s00228-018-2567-5.
Silva LT, Modesto ACF, Amaral RG, Lopes FM. Hospitalizations and deaths related to adverse drug events worldwide: systematic review of studies with national coverage. Eur J Clin Pharmacol. 2022;78:435–66. https://doi.org/10.1007/s00228-021-03238-2.
Shepherd G, Mohorn P, Yacoub K, May DW. Adverse drug reaction deaths reported in United States vital statistics, 1999–2006. Ann Pharmacother. 2012;46:169–75. https://doi.org/10.1345/aph.1P592.
Funahashi T, Koyama T, Hagiya H, Harada K, Iinuma S, Ushio S, et al. Population-based observational study of adverse drug event-related mortality in the super-aged society of Japan. Drug Saf. 2021;44:531–9. https://doi.org/10.1007/s40264-020-01037-9.
US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National action plan for adverse drug event prevention. 2014. https://health.gov/our-work/national-health-initiatives/health-care-quality/adverse-drug-events/national-ade-action-plan. Accessed 10 May 2023.
Duensing K, Twillman R, Ziegler S, Cepeda MS, Kern D, Salas M, et al. An examination of state and federal opioid analgesic and continuing education policies: 2016–2018. J Pain Res. 2020;13:2431–42. https://doi.org/10.2147/JPR.S267448.
Sommer H, Dwenger A. Action plan of the Federal Ministry of Health for improvement of medication safety in Germany: an inventory. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61:1062–5. https://doi.org/10.1007/s00103-018-2778-z.
Akishita M. Guidelines for medical treatment and its safety in the elderly. Nihon Ronen Igakkai Zasshi. 2007;44:31–4. https://doi.org/10.3143/geriatrics.44.31.
WHO. WHO Mortality Database. https://www.who.int/data/data-collection-tools/who-mortality-database. Accessed 24 June 2021.
Hohl CM, Karpov A, Reddekopp L, Doyle-Waters M, Stausberg J. ICD-10 codes used to identify adverse drug events in administrative data: a systematic review. J Am Med Inform Assoc. 2014;21:547–57. https://doi.org/10.1136/amiajnl-2013-002116.
United Nations. World population prospects 2019. https://www.un.org/development/desa/pd/news/world-population-prospects-2019-0. Accessed 20 June 2021.
Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–7.
Omar BA, Cynthia BP, Alan DL, Christopher JM, Rafael L, Mie I. Age standardization of rates: a new WHO standard. 2001. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf. Accessed 1 Dec 2022.
Cleveland WS, Devlin SJ. Locally weighted regression: an approach to regression analysis by local fitting. J Am Stat Assoc. 1988;83:596–610. https://doi.org/10.1080/01621459.1988.10478639.
Barco S, Mahmoudpour SH, Valerio L, Klok FA, Münzel T, Middeldorp S, et al. Trends in mortality related to pulmonary embolism in the European region, 2000–15: analysis of vital registration data from the WHO Mortality Database. Lancet Respir Med. 2020;8:277–87. https://doi.org/10.1016/S2213-2600(19)30354-6.
Kuklik N, Stausberg J, Jöckel KH. Adverse drug events in German hospital routine data: a validation of International Classification of Diseases, 10th Revision (ICD-10) diagnostic codes. PLoS ONE. 2017;12: e0187510. https://doi.org/10.1371/journal.pone.0187510.
CDC. NCHS. Provisional drug overdose death counts. In: National Vital Statistics System. Vital statistics rapid release. Surveillance activities. 2023. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed 23 Sep 2023.
FDA Adverse Event Reporting System (FAERS). U.S. Food & Drug Association. 2021. https://www.fda.gov/drugs/questions-and-answers-fdas-adverse-event-reporting-system-faers/fda-adverse-event-reporting-system-faers-public-dashboard. Accessed 24 Sep 2023.
VigiBase. Uppsala Monitoring Centre. 2021. https://who-umc.org/vigibase/vigibase-who-s-global-database/. Accessed 25 Sep 2023.
Chang AY, Cowling K, Micah AE, Chapin A, Chen CS, Ikilezi G, et al. Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050. Global Burden of Disease Health Financing Collaborator Network. Lancet. 2019;393:2233–60. https://doi.org/10.1016/S0140-6736(19)30841-4.
OECDiLibrary. Health at a glance 2021: OECD indicators. Pharmaceutical consumption. 2021. https://www.oecd-ilibrary.org/sites/5689c05c-en/index.html?itemId=%2Fcontent%2Fcomponent%2F5689c05c-en#. Accessed 25 Sep 2023.
Soldin OP, Mattison DR. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinet. 2009;48:143–57. https://doi.org/10.2165/00003088-200948030-00001.
Turner JP, Tannenbaum C. Older adults’ awareness of deprescribing: a population-based survey. J Am Geriatr Soc. 2017;65:2691–6. https://doi.org/10.1111/jgs.15079.
Hannah R, Max R. Opioids, cocaine, cannabis and illicit drugs; 2022. https://ourworldindata.org/illicit-drug-use. Accessed 14 May 2023.
Steinman MA, Miao Y, Boscardin WJ, Komaiko KD, Schwartz JB. Prescribing quality in older veterans: a multifocal approach. J Gen Intern Med. 2014;29:1379–86. https://doi.org/10.1007/s11606-014-2924-8.
Spencer MR, Miniño AM, Warner M. Drug overdose deaths in the United States, 2001–2021. NCHS Data Brief, vol 457. Hyattsville: National Center for Health Statistics; 2022. p. 1–8. https://doi.org/10.15620/cdc:122556. Accessed 14 May 2023.
Office for National Statistics. Deaths related to drug poisoning in England and Wales: 2019 registrations. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugpoisoninginenglandandwales/2019registrations. Accessed 25 May 2023.
Federal, Provincial, and Territorial Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and stimulant-related harms in Canada. 2023. https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/. Accessed 25 May 2023.
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Death rate maps & graphs. https://www.cdc.gov/drugoverdose/deaths/2013-2017-increase.html. Accessed 24 May 2023.
The European Monitoring Centre for Drugs and Drug Addiction; 2022: overdose deaths. Statistical Bulletin. https://www.emcdda.europa.eu/data/stats2022/drd_en.24 Accessed May 2023.
Chrzanowska A, Man N, Sutherland R, Degenhardt L, Peacock A. Trends in drug-induced deaths in Australia, 1997–2019. 2021. Drug trends bulletin series. https://ndarc.med.unsw.edu.au/resource-analytics/trends-drug-induced-deaths-australia-1997-2019. Accessed 22 May 2023.
Khan MAA, Hamid S, Babar ZU. Pharmacovigilance in high-income countries: current developments and a review of literature. Pharmacy. 2023;11:10. https://doi.org/10.3390/pharmacy11010010.
Gandhi TK, Weingart SN, Borus J, Seger AC, Peterson J, Burdick E, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556–64. https://doi.org/10.1056/NEJMsa020703.
Dequito AB, Mol PGM, van Doormaal JE, Zaal RJ, van den Bemt PM, Haaijer-Ruskamp FM, et al. Preventable and non-preventable adverse drug events in hospitalized patients: a prospective chart review in the Netherlands. Drug Saf. 2011;34:1089–100. https://doi.org/10.2165/11592030-000000000-00000.
Insani WN, Whittlesea C, Alwafi H, Man KKC, Chapman S, Wei L. Prevalence of adverse drug reactions in the primary care setting: a systematic review and meta-analysis. PLoS ONE. 2021;16: e0252161. https://doi.org/10.1371/journal.pone.0252161.
Hodkinson A, Tyler N, Ashcroft DM, Keers RN, Khan K, Phipps D, et al. Preventable medication harm across health care settings: a systematic review and meta-analysis. BMC Med. 2020;18:313. https://doi.org/10.1186/s12916-020-01774-9.
Acknowledgements
We thank Editage (www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the Japan Society for the Promotion of Science (KAKENHI Grant No. 22K10415). The sponsors had no role in the study design; in the collection, analysis and interpretation of the data; in the writing of the manuscript; and in the decision to submit the article for publication. All authors had full access to all of the data (including statistical reports and tables) in the study and take responsibility for the integrity and accuracy of the data.
Conflict of interest
Toshihiro Koyama, Shunya Iinuma, Michio Yamamoto, Takahiro Niimura, Yuka Osaki, Sayoko Nishimura, Ko Harada, Yoshito Zamami and Hideharu Hagiya have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
This study was approved by the Institutional Review Board of Okayama University Hospital (no. 2007-011) and performed following the Declaration of Helsinki. The requirement for informed consent was waived because of the retrospective nature and analysis of routinely collected data. Reporting of this study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and analysed during the current study are available from the corresponding author upon reasonable request. The corresponding author has full access to all the study data and takes final responsibility for the decision to submit this work for publication.
Code availability
The ICD-10 codes used in the study are provided as ESM.
Author contributions
TK conceived the study; TK, HH and SI designed the study and wrote the manuscript. TK, MY and SI performed the statistical analysis. TK, SI and TN performed the data processing. All authors interpreted the results and critiqued the manuscript. All authors gave final approval for publication of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koyama, T., Iinuma, S., Yamamoto, M. et al. International Trends in Adverse Drug Event-Related Mortality from 2001 to 2019: An Analysis of the World Health Organization Mortality Database from 54 Countries. Drug Saf 47, 237–249 (2024). https://doi.org/10.1007/s40264-023-01387-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-023-01387-0